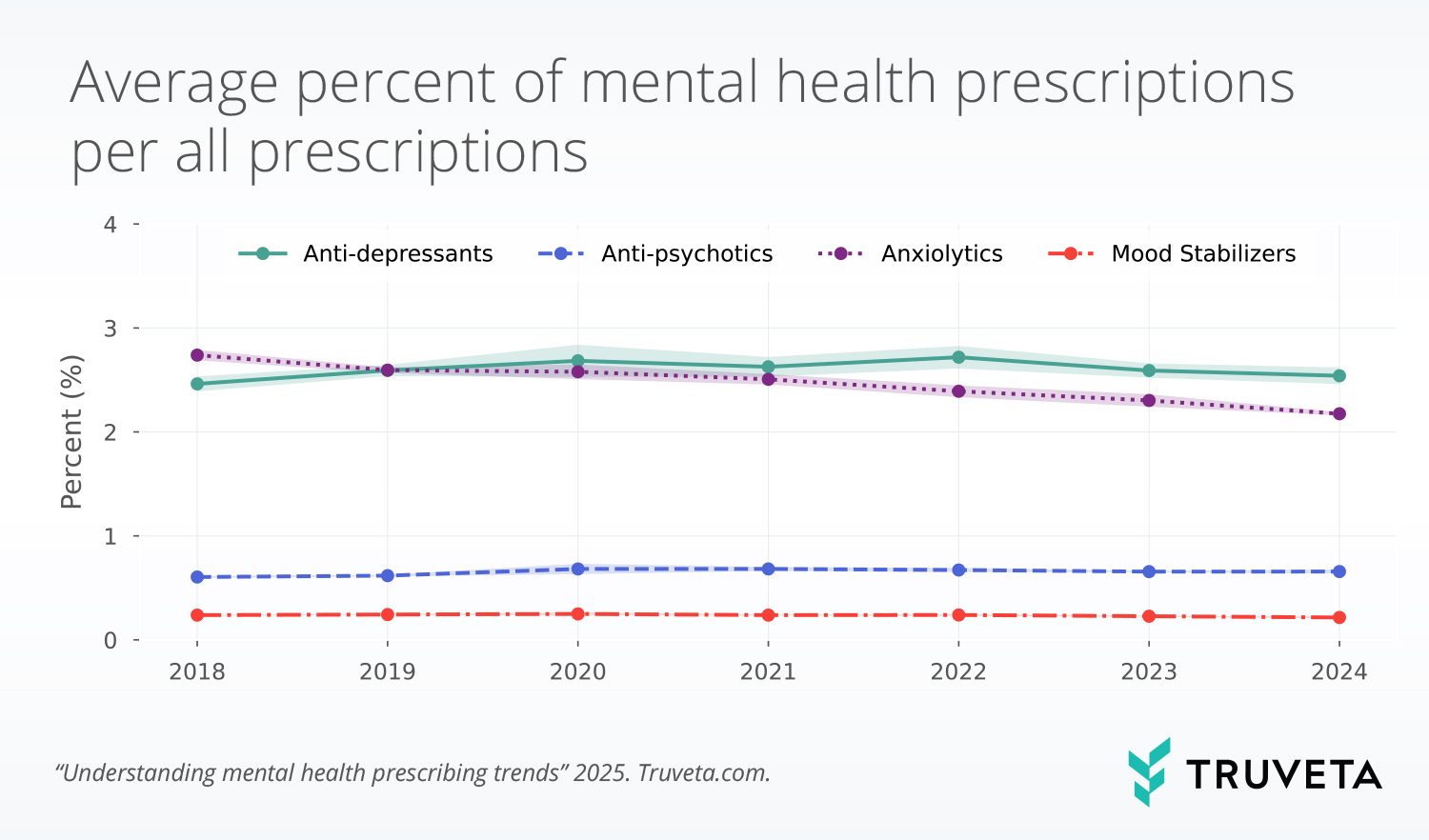
- Mental health prescribing remained relatively stable since 2018. Prescription rates for antidepressants, mood stabilizers, and antipsychotics peaked between 2020 and 2022 but have since stabilized or slightly declined compared to 2018 rates.
- Anxiolytic prescriptions have steadily decreased. The rate of prescriptions for anxiety medications, including benzodiazepines, has declined from 2.7% of all prescriptions in 2018 to 2.2% in 2024, this may align with increased awareness of their risks.
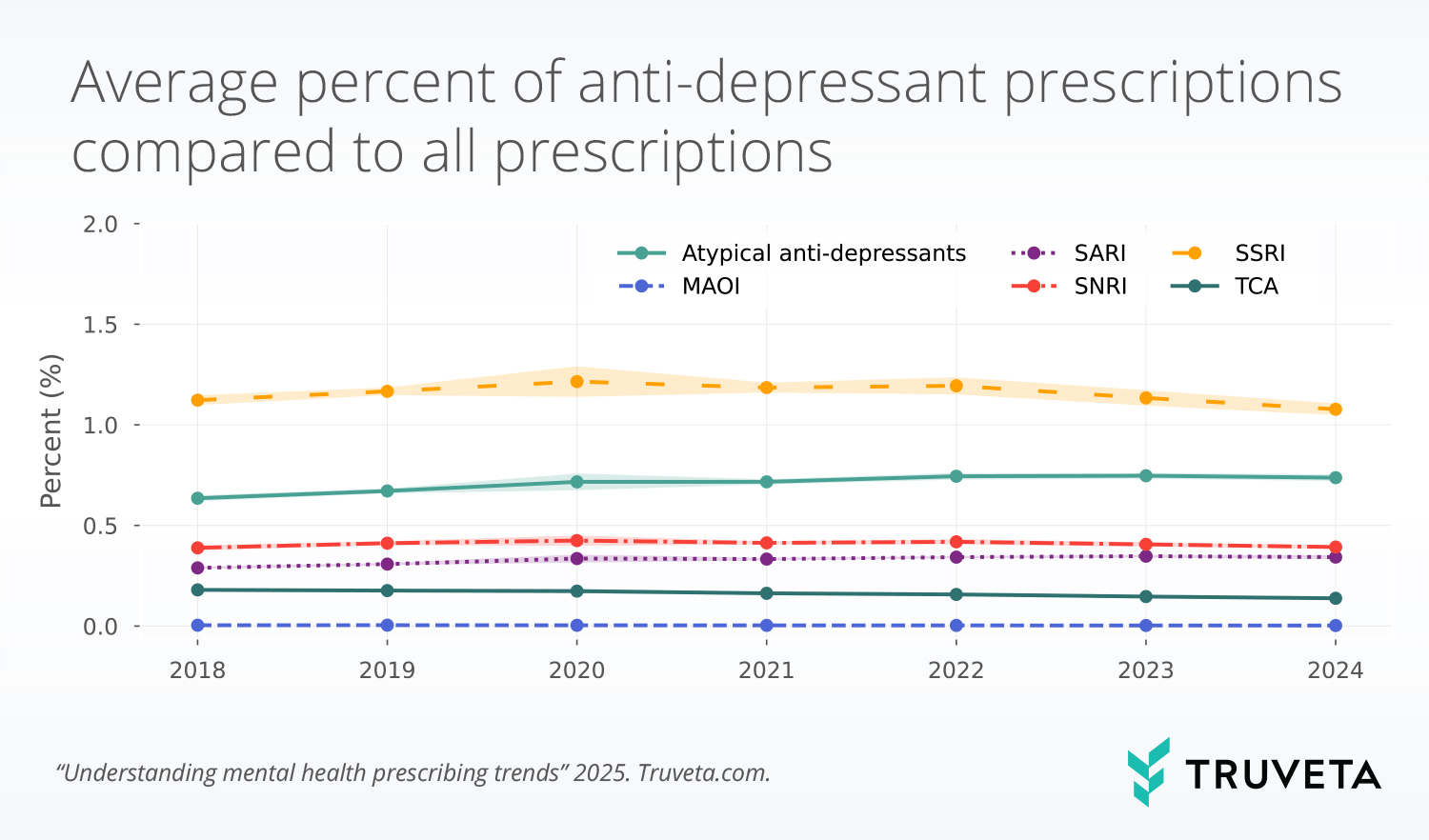
- Anti-depressants remain the most prescribed mental health medication. SSRIs account for nearly half of all antidepressant prescriptions. There are small changes in prescribing rates across the time period, however most drug classes peaked between 2020 and 2023 and have since decreased.
The conversation around mental health has gained momentum in recent years, with increased emphasis on reducing stigma (1), awareness (2), and the ability to talk about mental health topics (3). At the same time, the COVID-19 pandemic has increased the number of people with a variety of mental health conditions, creating a need for more mental health-related support (4–6). We’ve previously investigated trends in emergency department visits associated with mental health conditions, the trends in first-time anxiety diagnoses, and changes in diagnosis rates of ADHD over time.
Recently, literature has explored whether an increase in mental health awareness has led to an increase in people seeking care for mental health treatment (2, 7). Further, concerns around over-prescription, dependency, and the long-term effects of psychiatric medications have also fueled debates among healthcare professionals and the public alike. Examining prescription trends offers important insights into treatment patterns associated with mental health conditions.
We were curious to understand if there were changes in the rate of mental health prescriptions from 2018 to 2024.
Methods
Using a subset of Truveta Data, we included a population of patients who had a prescription between January 2018 and September 2024. For each month, we found the total number of prescriptions and the total prescriptions for four mental health drug classes: (1) anti-depressants, (2) anxiolytics, (3) anti-psychotics, and (4) mood stabilizers. We then calculated the monthly prescription rate for each mental health drug class relative to all prescriptions.
We further dug into drug classes within the anti-depressant prescription class. We included selective serotonin reuptake inhibitors (SSRI), serotonin-norepinephrine reuptake inhibitors (SNRI), serotonin antagonist and reuptake inhibitors (SARI), atypical anti-depressants (such as bupropion and trazodone), tricyclic anti-depressants (TCA), and monoamine oxidase inhibitors (MAOI) and evaluated potential changes overtime.
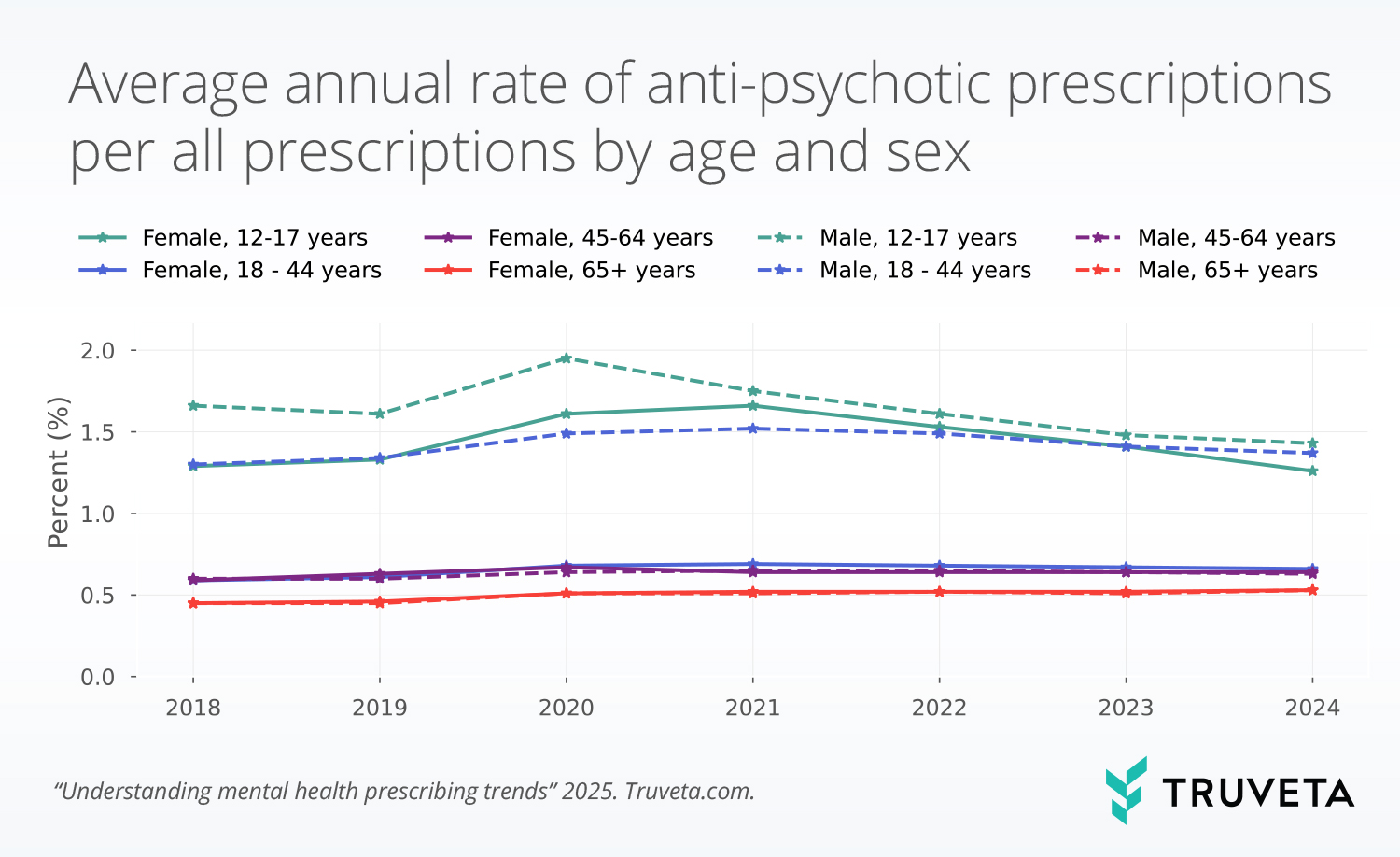
Additionally, we looked at the trends in rates of people receiving anti-psychotic medications by sex and four age groups.
Results
All drug classes
We found the rate of prescriptions to be highest for anxiolytics in 2018 and 2019 and for anti-depressants in all subsequent years. Since 2018, the rates of anxiolytics per all prescriptions has decreased. In 2018, 2.7% of all prescriptions were anxiolytics, however this has decreased to 2.2% so far in 2024. This is a decrease of 20.6% in anxiolytic prescription rates since 2018.
The rate of prescriptions for mood stabilizers, anti-psychotic, and anti-depressants reached their peak levels in 2020, 2021, and 2022, respectively. Since reaching their peaks, all rates have decreased slightly; across the full time period, the increases in each category are small. Mood stabilizers and anti-psychotics increased by less than 0.1 percentage points and anti-depressants increased by less than 0.3 percentage points.
Anti-depressants
In exploring anti-depressant prescriptions, SSRIs accounted for nearly half the prescriptions in this category (42%). The rate of most drug classes reached peak rates between 2019 and 2023 (SSRIs (2020), SNRIs (2020), SARIs (2023), MAOIs (2019)) and have decreased in most recent years , however the changes have been small for all drug classes. The absolute changes between 2018 and 2024 were greatest for SSRIs, but only changed by less than 0.14 percentage points. The rate of atypical anti-depressants increased slightly between 2018 (0.63%) and 2023 (0.75%), an increase of 17.6%. The rate of TCA prescriptions decreased slightly from 2018 (0.18%) to 2024 (0.14%), a decrease of 18.5%.
Anti-psychotics
Across the study period, the rates of anti-psychotics per all prescriptions were 1.2x higher, on average, for males compared to females. The rate of anti-psychotic prescriptions decreased with increasing age; 12–17-year-olds had the highest rates of anti-psychotic prescriptions followed by 18–44-year-olds. Within all age and sex groups, males 12-17 years old had the highest rate of anti-psychotic prescriptions across all years studied. The rate peaked in 2020 at 2.0%, but has since decreased to 1.4% in 2024. Interestingly, the rate for females aged 12-17 years old peaked in 2021, at 1.7% and then decreased to a rate of 1.3% in 2024.
Discussion
Our analysis of mental health prescription trends from 2018 to 2024 provides important insights into how prescribing patterns have changed over time. While increased mental health awareness and the heightened demand for care during the COVID-19 pandemic may have contributed to shifts in prescribing rates, our findings suggest that overall trends in mental health prescriptions have remained relatively stable, with only slight fluctuations in recent years. Our analysis showed a peak in prescription rates for mood stabilizers, anti-psychotics, and anti-depressants between 2020 and 2022, but rates have since shown a slight decline. These changes are relatively modest, with the overall proportion of mental health prescriptions remaining largely consistent over time.
Our findings also contribute to the ongoing discussion around whether increased mental health awareness has led to a rise in people seeking treatment and whether concerns around over-prescription are warranted (2, 7). While there was a slight increase in the rate of mental health prescriptions during the peak years of the COVID-19 pandemic, the subsequent stabilization and decrease suggests that the rise was likely a temporary response to heightened mental health needs rather than a long-term shift toward higher prescribing rates. Additionally, the decline in anxiolytic prescriptions since 2018 suggests that healthcare providers may be moving toward alternative treatments for anxiety disorders, such as psychotherapy or non-benzodiazepine medications. Benzodiazepines are a class of drugs within the anxiolytic class. Prior to 2015 there was a reported increase in use of benzodiazepines in outpatient settings (8); however, since then new guidelines from the CDC on when to prescribe benzodiazepines were released (9) and the FDA has required label changes to describe the risks associated with the drugs (10). Overall, there is also an increased awareness of the risks of using this class of drugs (11). Our results show the rates of prescribing anxiolytic have decreased since 2018 compared to all other prescriptions, and a decrease in benzodiazepines may be contributing.
We see age and sex differences in prescribing trends for anti-psychotic medications. The rates in our analysis are highest for males and specifically younger males (aged 12-17 years old). Schizophrenia is one condition anti-psychotic medications are used to treat. The differences by sex shown here are similar to the sex distributions of people with schizophrenia (12). Recently we showed the rate of emergency department (ED) encounters related to schizophrenia by age and sex.
These findings highlight the importance of continued research into prescribing trends, particularly as mental health awareness continues to grow and new treatment options emerge. Future studies should explore additional factors influencing prescription rates, such as demographic differences, healthcare access, and the impact of non-pharmacological treatments. Understanding these patterns can help guide evidence-based prescribing practices and ensure that mental health care remains both accessible and effective.
There are a few limitations with this analysis. First, we calculate the rate of prescriptions, not people. Second, we did not take into account the diagnoses associated with prescriptions for each drug class. Many of these drug classes are used to treat multiple conditions, and we did not determine which conditions were associated with each drug class. Finally, we included data through September 2024; however, we present 2024 rates. Caution should be taken when interpreting these data as they may change.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on October 8, 2024.
Citations
- A. Hajizadeh, H. Amini, M. Heydari, F. Rajabi, How to combat stigma surrounding mental health disorders: a scoping review of the experiences of different stakeholders. BMC Psychiatry 24, 782 (2024).
- N. Haslam, J. S. Tse, Public awareness of mental illness: Mental health literacy or concept creep? Australas Psychiatry, 10398562241292202 (2024).
- CVS Health, CVS Health / Morning Consult survey finds mental health concerns increase substantially among Americans of all backgrounds (2022). https://www.cvshealth.com/news/mental-health/cvs-health-morning-consult-survey-finds-mental-health-concerns.html.
- World Health Organization, “Mental health and COVID-19: early evidence of the pandemic’s impact: scientific brief, 2 March 2022” (World Health Organization, 2022); https://www.who.int/publications/i/item/WHO-2019-nCoV-Sci_Brief-Mental_health-2022.1.
- World Health Organization, COVID-19 pandemic triggers 25% increase in prevalence of anxiety and depression worldwide (2022). https://www.who.int/news/item/02-03-2022-covid-19-pandemic-triggers-25-increase-in-prevalence-of-anxiety-and-depression-worldwide.
- B. W. J. H. Penninx, M. E. Benros, R. S. Klein, C. H. Vinkers, How COVID-19 shaped mental health: from infection to pandemic effects. Nat Med 28, 2027–2037 (2022).
- L. Foulkes, J. L. Andrews, Are mental health awareness efforts contributing to the rise in reported mental health problems? A call to test the prevalence inflation hypothesis. New Ideas in Psychology 69, 101010 (2023).
- S. D. Agarwal, B. E. Landon, Patterns in Outpatient Benzodiazepine Prescribing in the United States. JAMA Netw Open 2, e187399 (2019).
- D. Dowell, T. M. Haegerich, R. Chou, CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recomm. Rep. 65, 1–49 (2016).
- U.S. Food & Drug Administration, “FDA Requiring Labeling Changes for Benzodiazepines” (2020); https://www.fda.gov/news-events/press-announcements/fda-requiring-labeling-changes-benzodiazepines.
- National Alliance on Mental Illness, Risks of Benzodiazepines (2024). https://www.nami.org/about-mental-illness/treatments/mental-health-medications/risks-of-benzodiazepines/.
- X. Li, W. Zhou, Z. Yi, A glimpse of gender differences in schizophrenia. Gen Psych 35, e100823 (2022).