- For patients coming into the emergency department (ED) with nausea/vomiting or dehydration, patients are half as likely to receive IV fluids starting 10 days after the hurricane compared to prior to Hurricane Helene. We expect these numbers to continue to decrease.
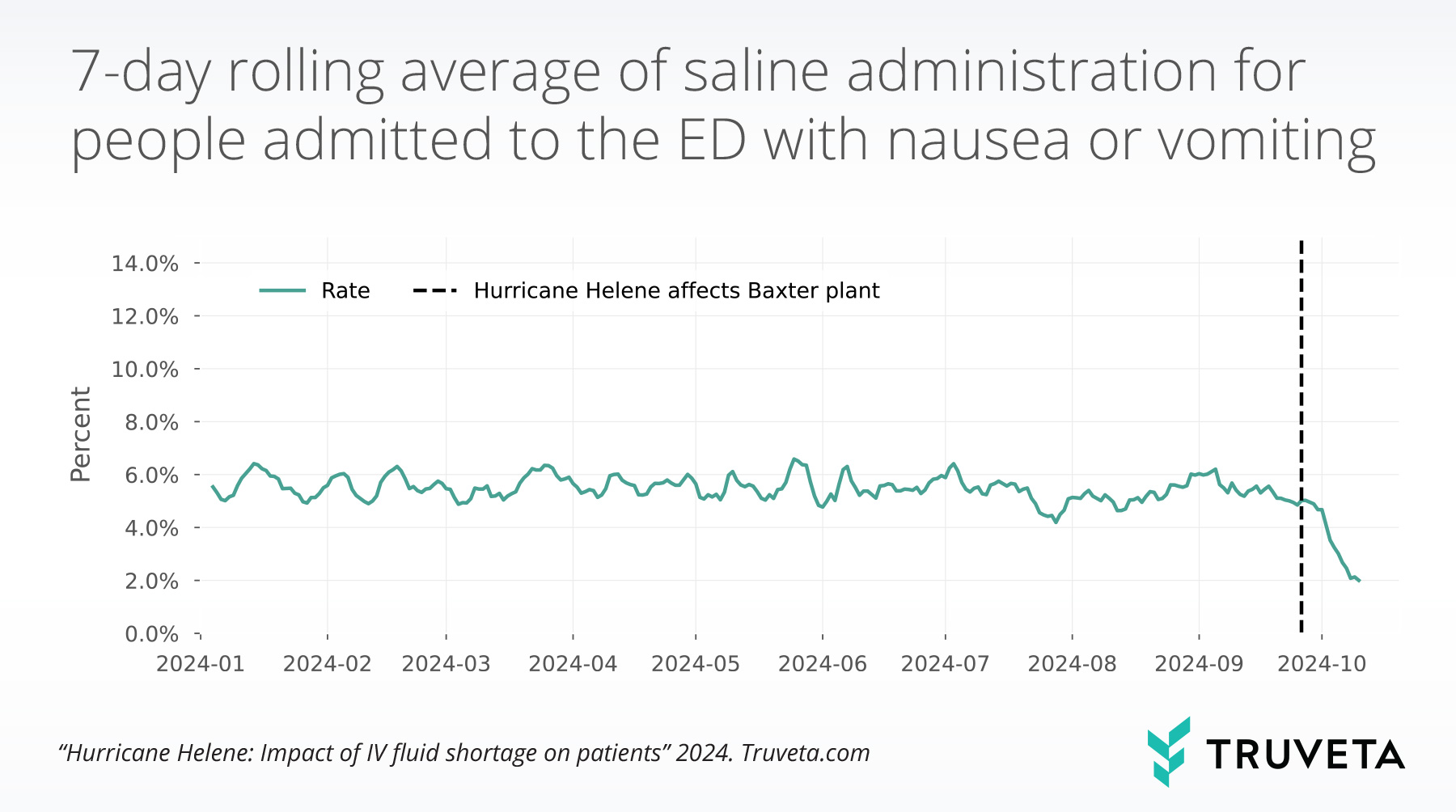
- The average rate of saline administration for patients in the ED with nausea or vomiting has decreased from 5.5% prior to Hurricane Helene to 2.0% ten days after, a decrease of 170.9 percentage points.
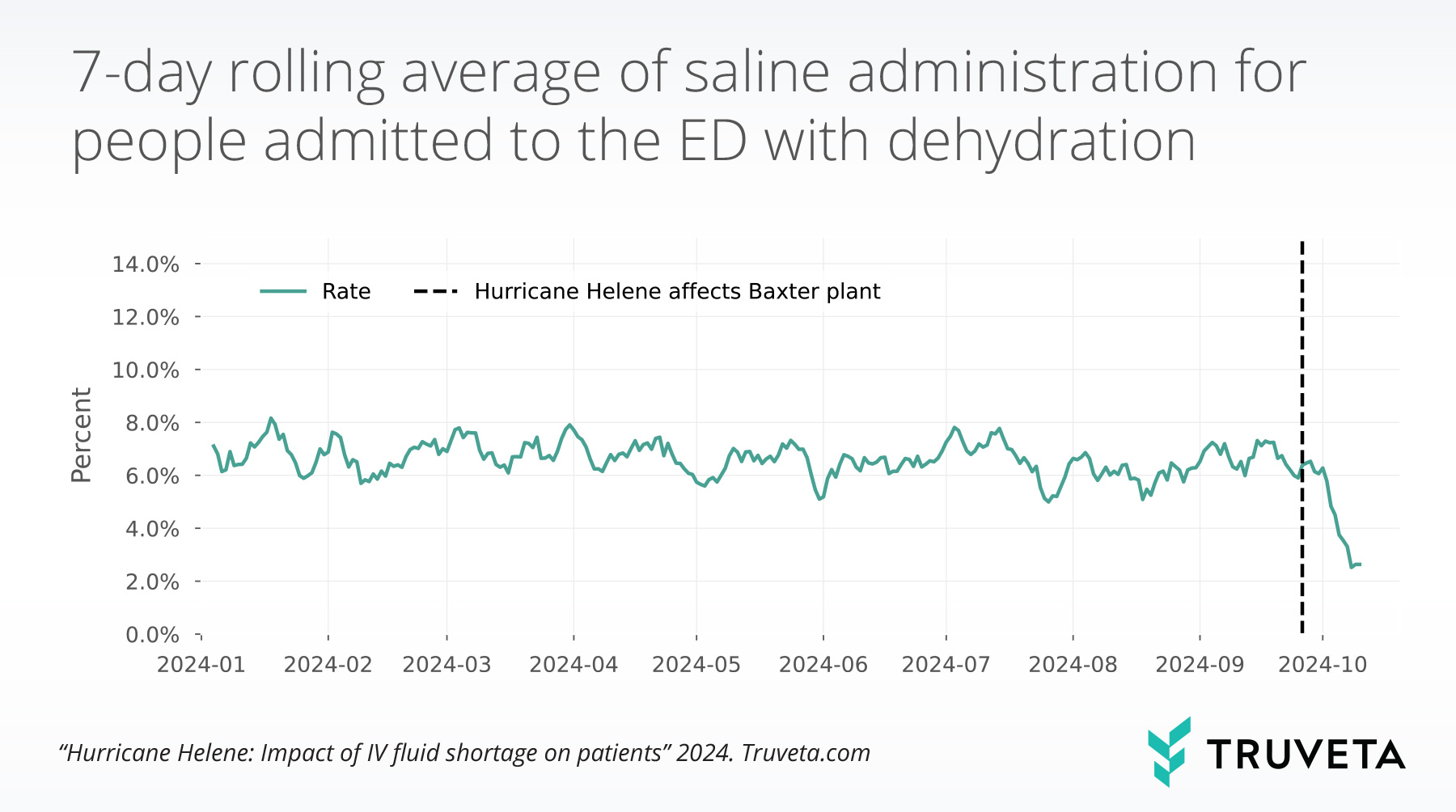
- Similarly, the average rate of saline administration among patients admitted to the ED with dehydration decreased from 6.6% before the hurricane to 2.5% the ten days after, a decrease of 162.5 percentage points.
On September 26, 2024 Hurricane Helene made landfall, damaging a manufacturing plant that produces IV fluids (Lupkin, 2024). This has intensified an already existing shortage of these fluids (U.S. Food & Drug Administration, 2024).
There are many potential impacts of reduced availability of IV fluids. For example, saline is commonly used to rehydrate patients, restore blood volume, manage blood pressure, and as support during surgery. Sufficient hydration is associated with shorter hospital stays and reduced postoperative complications (Bruno et al., 2021; Gawronska et al., 2022). The impacts of the decrease in saline available could be wide stretching and may only be just beginning to be felt.
To understand how the damage to the Baxter manufacturing plant might have impacted patient care, Truveta Research explored how the rate of saline administration in the emergency department (ED) for nausea/vomiting or dehydration has changed since Hurricane Helene further worsened the shortage.
You can also view this study directly in Truveta Studio.
Methods
Using a subset of Truveta Data we included people twelve and older who had an emergency department (ED) encounter and presented with nausea/vomiting or dehydration between January 1, 2024 and October 13, 2024.
We identified patients who received either 1000mL or 500mL saline fluids within the same ED encounter. We calculated the daily rate of saline administrations per people admitted to the ED with nausea/vomiting or dehydration. We also investigated the rates across different age groups (12-17, 18-29, 30-44, 45-64, and 65+ years of age).
Results
We examined 277,500 ED encounters for patients presenting with nausea or vomiting and 68,246 ED encounters for patients presenting with dehydration between January 1, 2024 and October 13, 2024.
People admitted to the ED with nausea or vomiting
Before Hurricane Helene’s landfall, the average rate of saline administration for patients in the ED with nausea or vomiting was 5.5±1.1%. However, 10 days later, the rate dropped to 2.0±0.5%, representing a decrease of 170.9 percentage points.
This trend was consistent across all age groups studied.
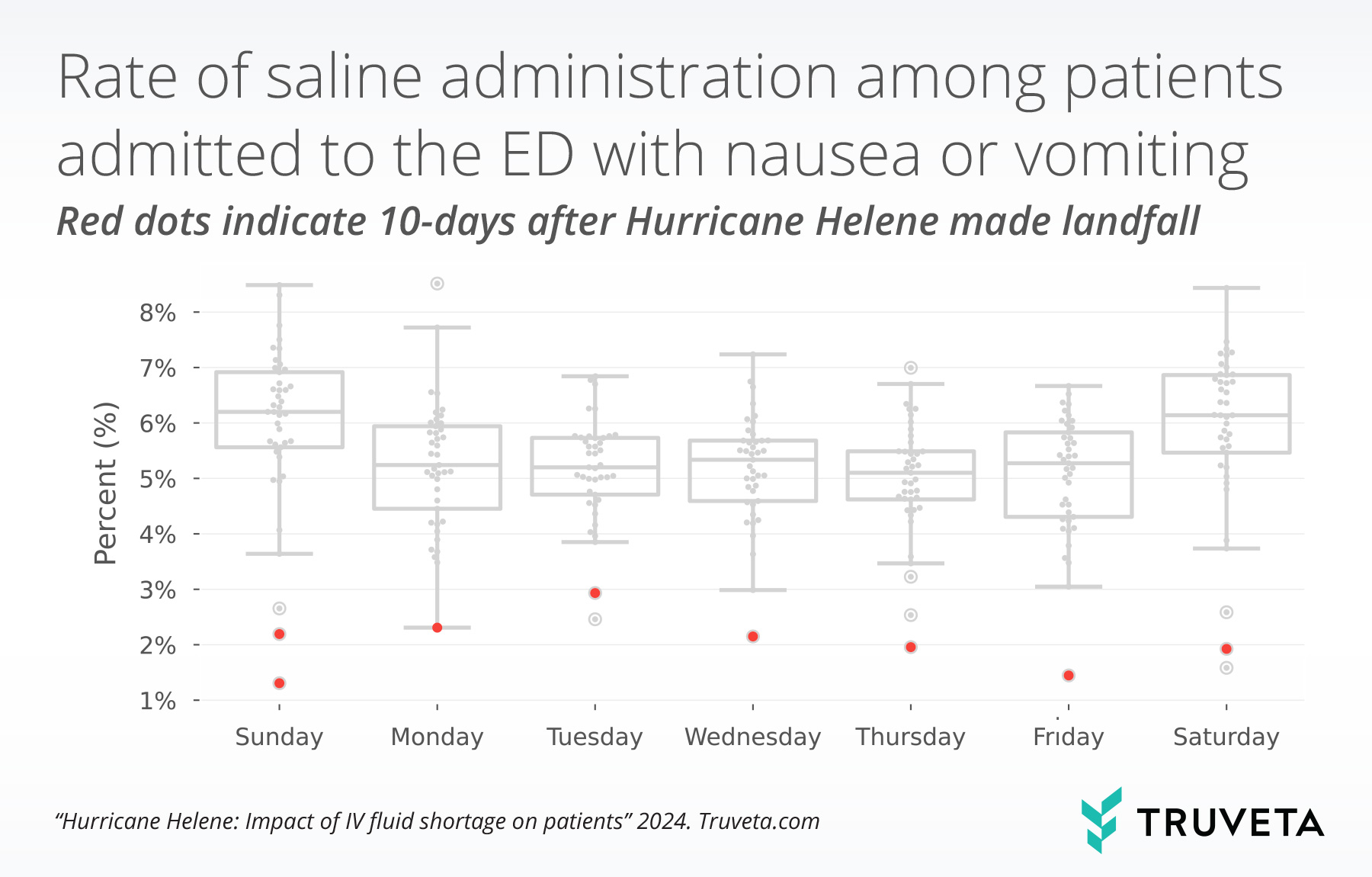
There is variation in the rate of saline administration among patients admitted to the ED with nausea or vomiting by day of the week. The graph below shows these trends. Prior to Hurricane Helene making landfall the average rates of saline administration were highest on weekend days (Saturday and Sunday).
The red dots indicate the average rates of saline administration by day of the week, starting 10 days after Hurricane Helene made landfall (e.g., on or after October 6, 2024). The red dots within the figure below suggests that the average rate of saline administration was substantially lower on every day of the week 10 days after hurricane Helene made landfall, compared with those average rates on the same day of the week before the hurricane made landfall.
People admitted to the ED with dehydration
The average rate of saline administration among patients admitted to the ED with dehydration was 6.6±1.6% prior to Hurricane Helene making landfall. Ten days after the rate dropped to 2.5±0.9%; representing a decrease of 162.5 percentage points.
This trend was consistent across all age groups studied.
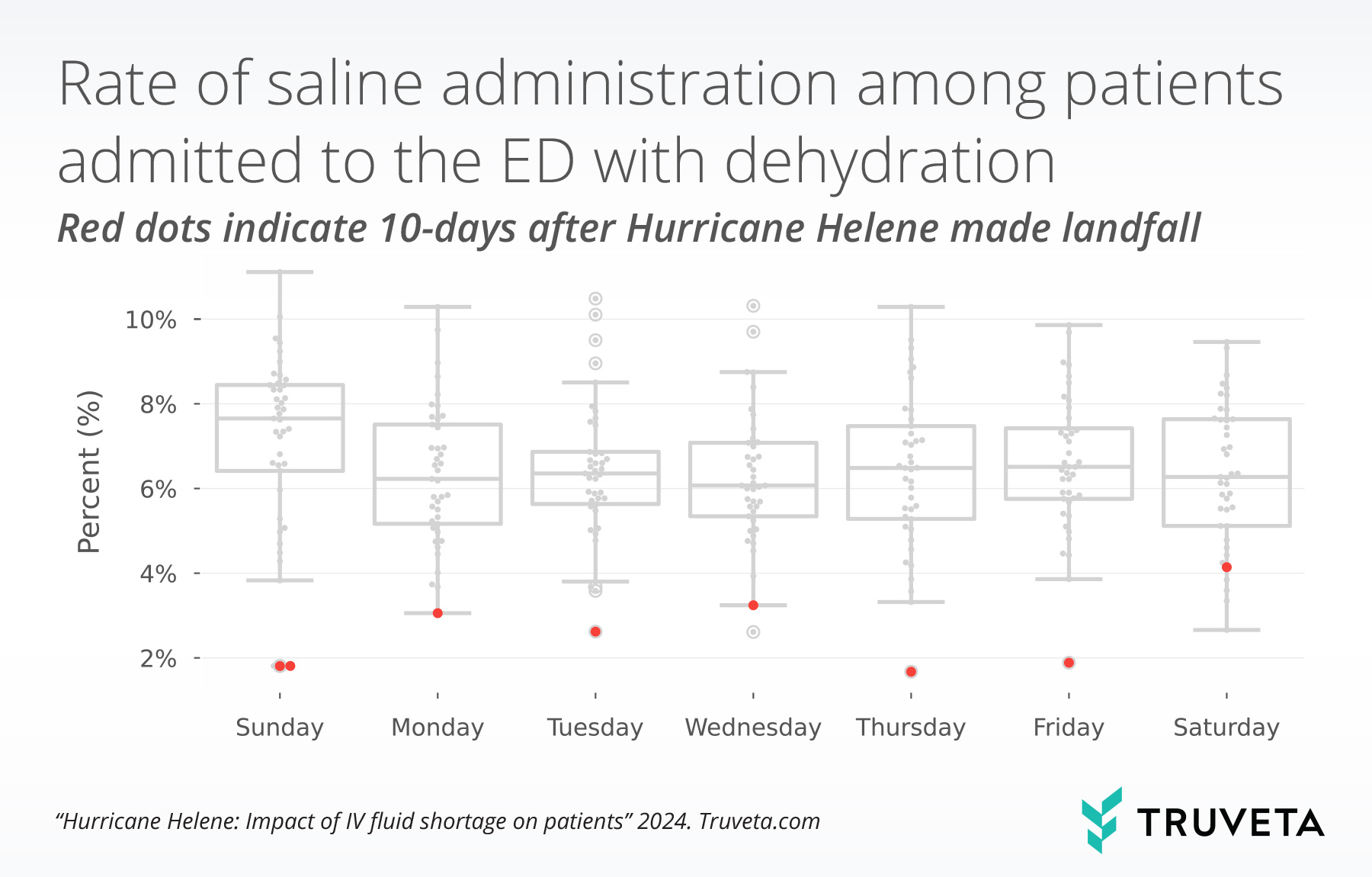
Similar to the rates of saline administration for nausea or vomiting, we also see variation in the rate of people who receive saline when admitted to the ED for dehydration by day of the week. Saturday had the highest mean rate of saline administration in this population.
The graph below shows these trends. The red dots indicate the average rates of saline administration by day of the week, starting 10 days after Hurricane Helene made landfall (e.g., on or after October 6, 2024).
Discussion
In this analysis we see patients admitted to the ED with nausea/vomiting or dehydration to be half as likely to receive saline fluids 10 days after Hurricane Helene made landfall, compared to before the Hurricane. With the recovery efforts still underway in western North Carolina and expected to continue through the end of the year (Kansteiner, 2024), the saline shortage is expected to continue. We anticipate this to lead to even further decreases in the rates shown here.
Patients who are not receiving saline fluids in this population may instead be given anti-nausea medications or oral rehydration therapy (i.e., asked to drink electrolyte beverages such as Gatorade) (Lupkin, 2024). The shortage could impact health systems in other ways such as reduced rates of elective surgeries (Murphy, 2024) or increases in additional medications given to manage patients with high blood pressures. Additionally, health system size may impact their ability to access and re-distribute available saline fluids, making patients in rural areas more impacted than patients in urban areas. The impacts on patient care are unknown and will likely continue to intensify as the shortage increases.
This analysis does not come without limitations; first, the population we included was patients over 12 years of age. However, for all age groups included in this analysis we saw decreased rates in the administration of saline. Second, while the known prevalence of saline use in EDs isn’t well described in the literature, this analysis may under capture the total number of patients who received saline fluids. However, we wouldn’t expect this to impact pre- and post- hurricane periods differently.
To the best of our knowledge, this is the first analysis showing a change to patient care following damage to the Baxter manufacturing plant.
These are preliminary research findings and not peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on October 23, 2024. You can also view this study directly in Truveta Studio.
Citations
Bruno, C., Collier, A., Holyday, M., & Lambert, K. (2021). Interventions to Improve Hydration in Older Adults: A Systematic Review and Meta-Analysis. Nutrients, 13(10), 3640. https://doi.org/10.3390/nu13103640
Gawronska, J., Koyanagi, A., López Sánchez, G. F., Veronese, N., Ilie, P. C., Carrie, A., Smith, L., & Soysal, P. (2022). The Prevalence and Indications of Intravenous Rehydration Therapy in Hospital Settings: A Systematic Review. Epidemiologia, 4(1), 18–32. https://doi.org/10.3390/epidemiologia4010002
Kansteiner, F. (2024, October 9). Baxter offers recovery timeline after major IV fluid plant closure due to Hurricane Helene. https://www.fiercepharma.com/pharma/baxter-offers-recovery-timeline-after-major-iv-fluid-plant-closure-due-hurricane-helene
Lupkin, S. (2024, October 4). Storm damage closes N.C. factory that makes vital hospital supplies. NPR. https://www.npr.org/sections/shots-health-news/2024/10/04/g-s1-26383/iv-fluids-shortage-baxter-hurricane-helene
Murphy, T. (2024, October 22). Hospitals’ IV fluid shortage may impact surgeries for weeks. ABC News. https://abcnews.go.com/Health/wireStory/hospitals-iv-fluid-shortage-impact-surgeries-weeks-115027715
U.S. Food & Drug Administration. (2024, October 25). Hurricane Helene: Baxter’s manufacturing recovery in North Carolina. https://www.fda.gov/drugs/updates-2024-hurricane-season/hurricane-helene-baxters-manufacturing-recovery-north-carolina