- The analysis was based on a sample of 17,501,982 patients from January 2018 to May 2024. During the study period, 9,271 patients were tested (using CPT code 93922) for the first time and had a diagnosis of peripheral vascular disease/peripheral artery disease (PVD/PAD) within 1 month before or after the test.
- Overall, trends in testing and diagnosis of PVD/PAD increased considerably from 7.0 per 100,000 patients in January 2018 to 14.7 per 100,000 in March 2023, then started to decline to 9.6 per 100,000 in May 2024. Much of the increase was primarily driven by white patients, Hispanic patients, and those living in the northeast region.
- Throughout the study period, higher incidence was observed for Medicare-eligible patients (ages 65+), male sex, white race, non-Hispanic ethnicity, and patients living in the northeast region.
- While the incidence of testing and diagnosis of PVD/PAD in an inpatient setting declined during the study period (4.3 per 100,000 patients in January 2018 vs. 2.1 in May 2024), the incidence in an outpatient setting accelerated over the same period (2.8 per 100,000 patients in January 2018 vs. 6.2 in May 2024).
Peripheral vascular disease (PVD) is a disorder of blood vessels outside of the heart and brain, affecting the extremities and organs. PVD (commonly also interchanged with peripheral artery disease or PAD) causes the narrowing, spasming, or blocking of blood vessels, and when left untreated, may require amputation. There are non-invasive tests that can be used to diagnose PVD/PAD, in addition to several treatment options.
PVD/PAD tends to impact adults over the age of 50, more men than women, and studies have shown that PVD/PAD disproportionately impacts both Black or African American (henceforth referred to as Black) and Hispanic or Latino individuals (Virani, et al, 2021; Cartwright, et al, 2022).
In partnership with STAT News, Truveta Research explored trends in the incidence of testing and diagnosis of PVD/PAD among U.S. patients aged 50 years and older from 2018 to 2024.
Methods
In each month from January 2018 to May 2024, we identified patients considered “at-risk” for the incidence of PVD/PAD – including patients with at least one valid inpatient or outpatient encounter, aged 50 years or older at the time of their encounter, no prior testing related to PVD/PAD, and had any inpatient or outpatient encounter in the prior 12 months.
We then ascertained the proportion of at-risk patients in a given month who had any test associated with CPT code 93922 – limited bilateral noninvasive physiologic studies of upper or lower extremity arteries – and any diagnosis of PVD/PAD within a window of 1 month before or after the test. This test is performed to establish the level and/or degree of PVD/PAD. The CPT code covers various tests (i.e., plethysmography, oxygen tension measurements, and Doppler waveform analysis) that quantify the rate of blood flow and assess the presence of blockage in the extremity arteries.
We used descriptive statistics to examine trends in the incidence of testing and diagnosis of PVD/PAD. The monthly incidence rate (per 100,000 at-risk patients) was calculated by dividing the number of patients with the test of interest by the number of at-risk patients. We stratified the analysis according to demographics (age, sex, race, and ethnicity), US geographical region, and place of service of the test (i.e., inpatient or outpatient setting).
Results
Using a subset of Truveta data, we identified 17,501,982 at-risk patients from January 2018 to May 2024. During the study period, 9,271 patients had a test for the first time and a diagnosis of PVD/PAD within 1 month before or after the test. Table 1 describes characteristics of these 9,271 patients with incident testing and diagnosis of PVD/PAD.
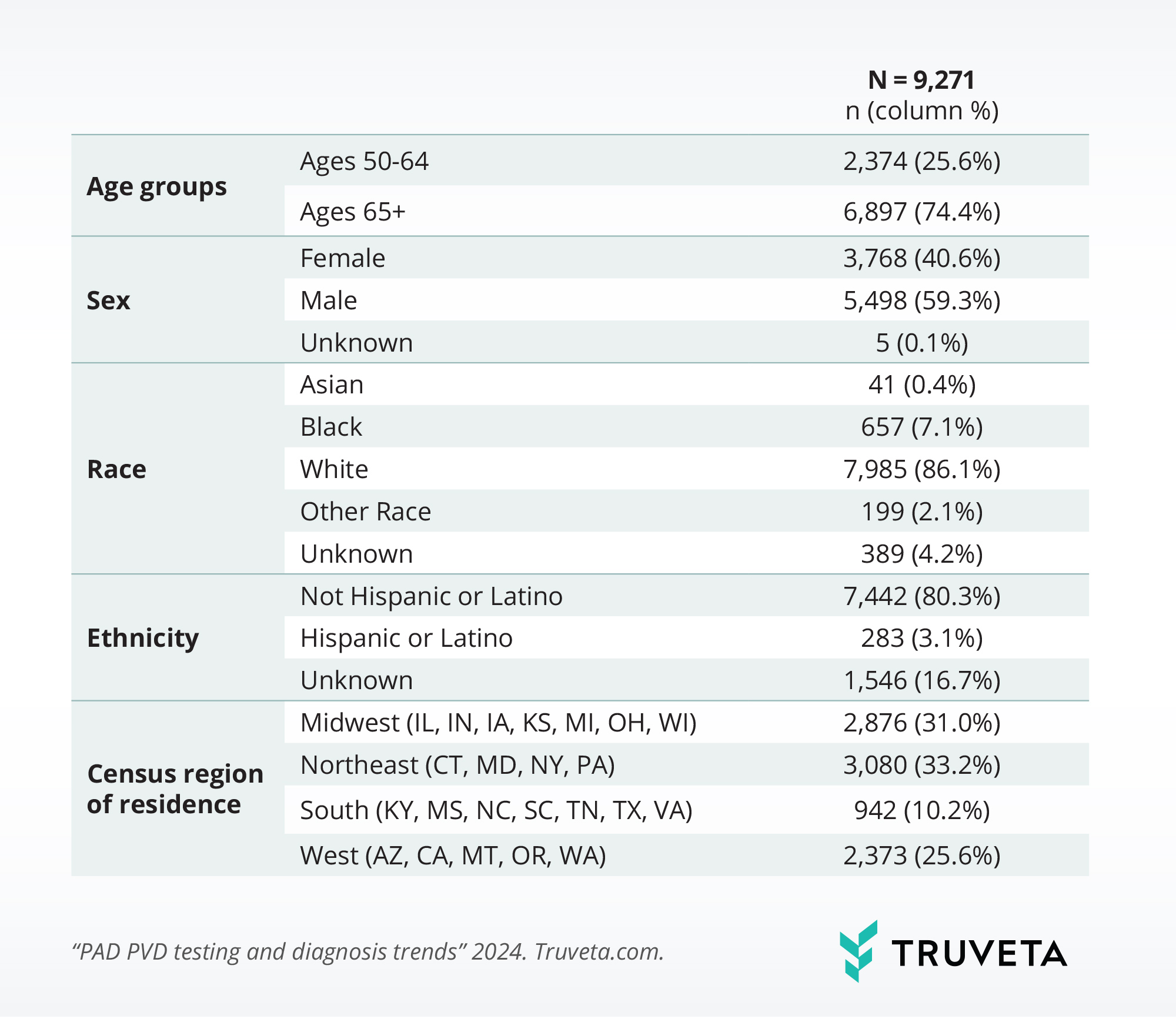
Table 1: Characteristics of patients with incident testing and diagnosis of PVD/PAD, 2018-2024
Figure 1 depicts trends in the incidence of testing and diagnosis of PVD/PAD from 2018 to 2024. Overall, trends in the incidence increased considerably from 7.0 per 100,000 patients in January 2018 to 14.7 per 100,000 in March 2023, and then started to decline to 9.6 per 100,000 in May 2024 (Figure 1a). Patients aged 65 years or older, male patients, white patients, non-Hispanic patients, and patients living in the northeast region had a higher incidence rate than that of their peers (Figures 1b to 1f). Much of the increase was primarily driven by white patients, Hispanic or Latino patients, and those living in the northeast region (see Table 2 for changes in the incidence rate between January 2018 and May 2024 by population subgroups).
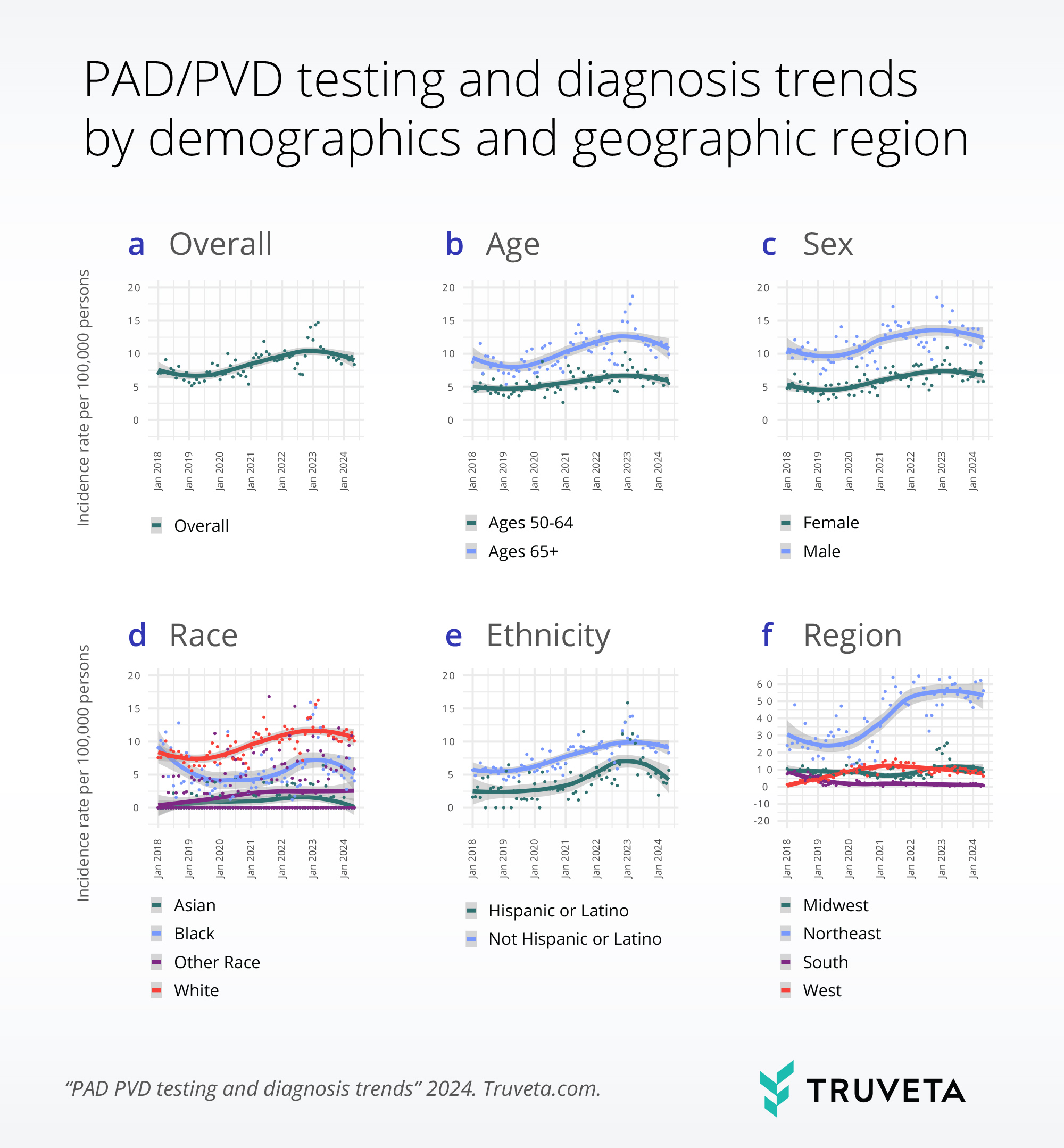
Figure 1: Trends in the incidence of testing and diagnosis of PVD/PAD, overall and by selected patient characteristics, 2018-2024.
Note: Gray areas depict 95% confidence interval around the fitted line. Trends in the incidence of testing and diagnosis of PVD/PAD were smoothed using locally estimated scatterplot smoothing (LOESS), a non-parametric regression method that combines multiple linear regression models in a k-nearest-neighbor-based meta model.
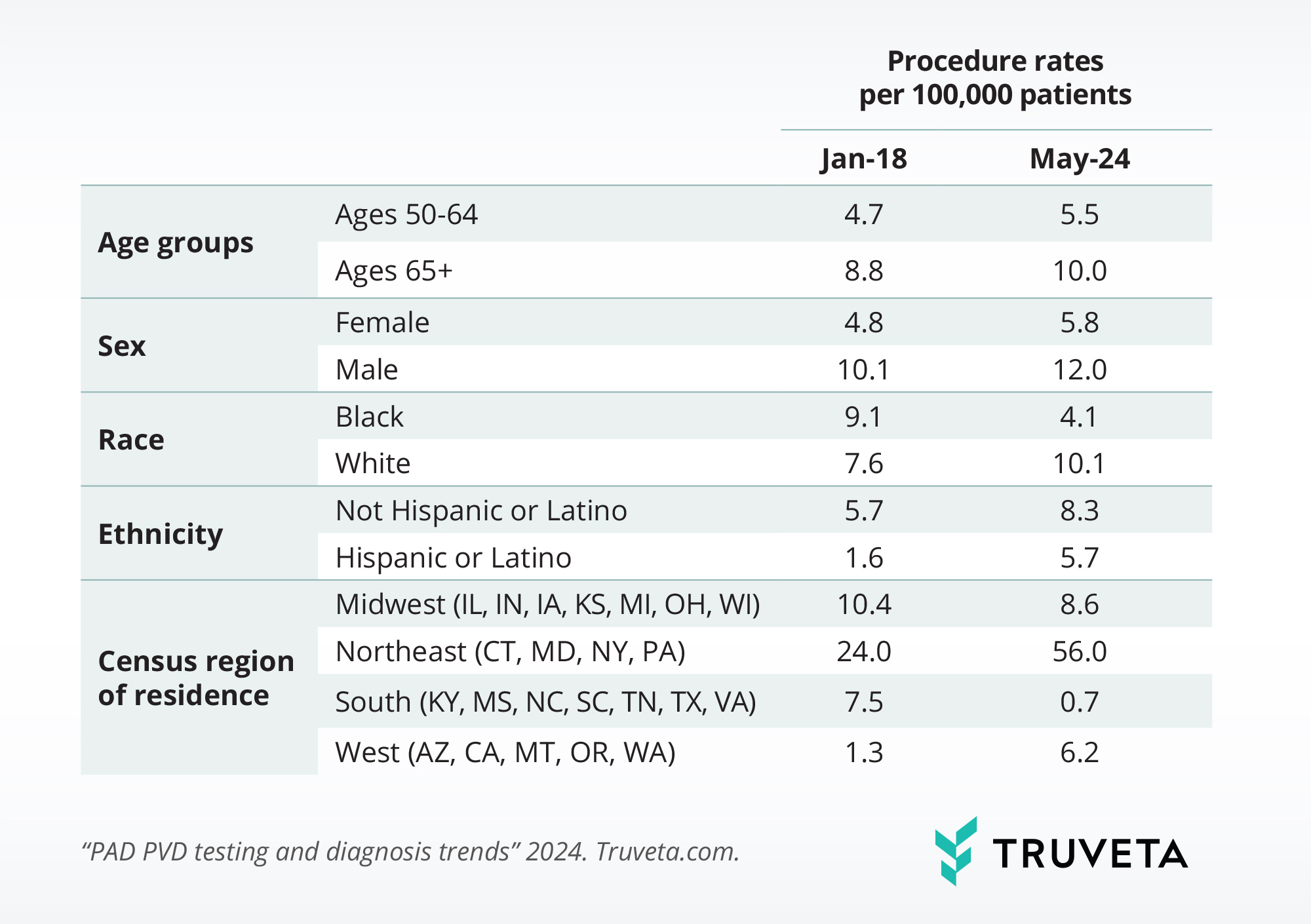
Table 2: Changes in the incidence rate of testing and diagnosis of PVD/PAD between January 2018 and May 2024 by population subgroups.
Figure 2 presents trends in the incidence of testing and diagnosis of PVD/PAD by outpatient or inpatient setting. While the incidence rate in an inpatient setting declined during the study period (4.3 per 100,000 patients in January 2018 vs. 2.1 in May 2024), that in an outpatient setting accelerated over the same period (2.8 per 100,000 patients in January 2018 vs. 6.2 in May 2024).
Notably, the incidence rate in an inpatient setting was higher than that in an outpatient setting at the beginning of the study period, but lower by the end of the study period.
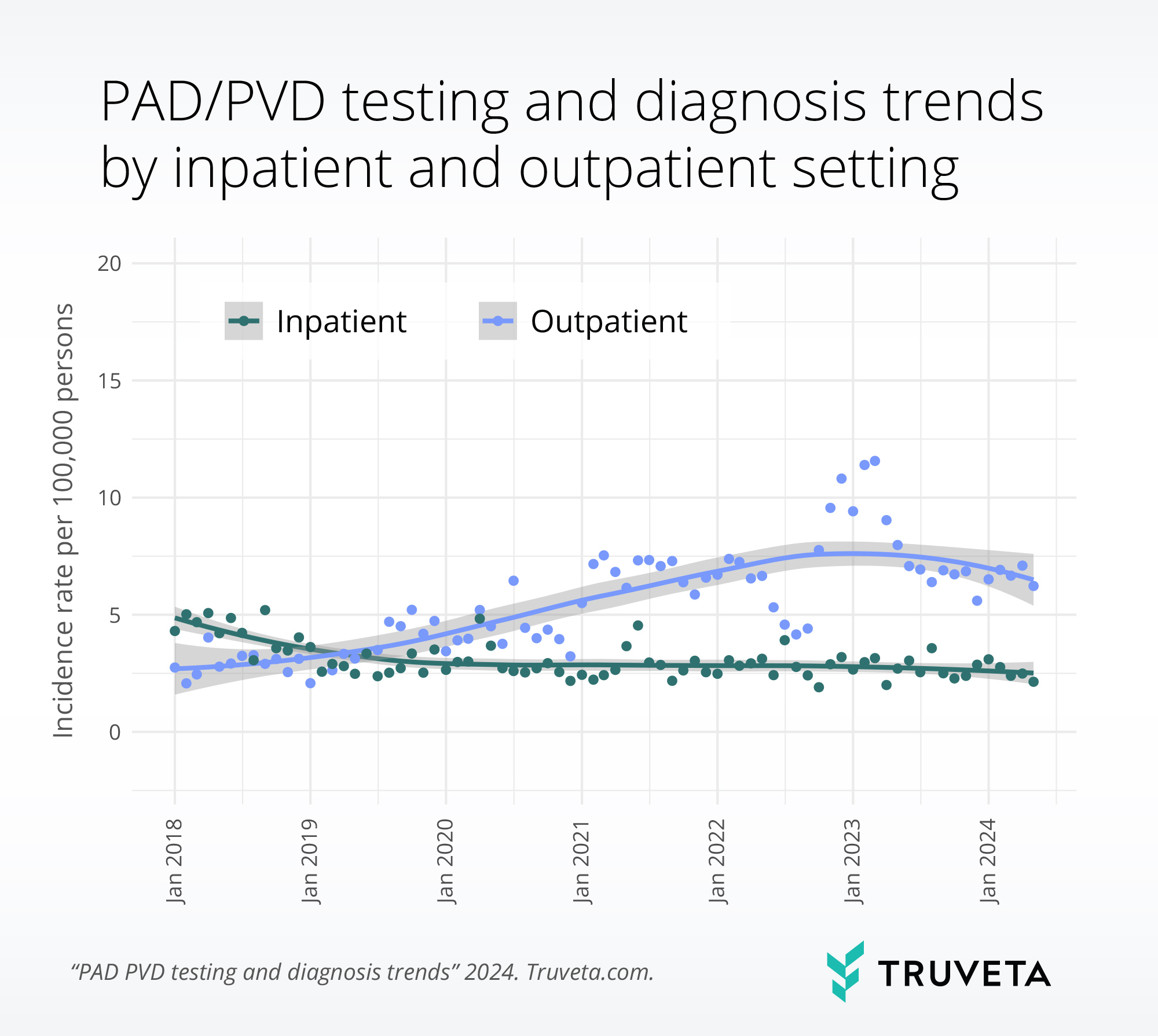
Figure 2: Trends in the incidence rate of testing and diagnosis of PVD/PAD, by place of service, 2018-2024.
Note: Gray areas depict 95% confidence interval around the fitted line. Trends in the incidence of testing and diagnosis of PVD/PAD were smoothed using locally estimated scatterplot smoothing (LOESS), a non-parametric regression method that combines multiple linear regression models in a k-nearest-neighbor-based meta model.
Discussion
This analysis showed that the incidence rates of testing (using CPT code 93922) and diagnosis of PVD/PAD increased from 2018 to 2023, then started to decline in the spring of 2024. The findings also highlighted the demographic and geographic disparities in testing and diagnosis of PVD/PAD. For instance, the rates of testing for the diagnosis of PVD/PAD were higher among white and non-Hispanic patients, despite PVD/PAD disproportionately impacting Black and Hispanic or Latino individuals (Cartwright, et al, 2022). Future studies should investigate whether and how such disparities in testing and diagnosis may translate to widening disparities in health outcomes and treatment initiation. Furthermore, more research is merited to understand specific factors influencing these testing and diagnosis trends.
As with any study, there are a few limitations with this analysis. For example, this study didn’t capture events that occurred outside of Truveta member health systems, and thus may miss testing that occurred or not include patients who received care in other settings.
These are preliminary research findings and have not been peer reviewed. Data are constantly changing and updating. These findings are consistent with data accessed on July 16, 2024.
You can view this study — including data definitions and all associated files — in Truveta Studio.
Citations
- Virani, Salim S., et al. “Heart disease and stroke statistics—2021 update: a report from the American Heart Association.” Circulation8 (2021): e254-e743. https://www.ahajournals.org/doi/10.1161/CIR.0000000000000950
- Cartwright, B., et al. “Peripheral artery disease treatment and outcomes: Disparities in frequency and revascularization procedures and incidence of adverse outcomes.” Truveta. September 2022. Peripheral artery disease treatment and outcomes: Disparities in frequency of revascularization procedures and incidence of adverse outcomes – Truveta