- Truveta Research in collaboration with a Harvard Medical School researcher explore use of obesity treatments in youth before and after new comprehensive guidelines for obesity management were published by the American Academy of Pediatrics (AAP).
- In a study of 329,357 patients aged 8 to 17, Truveta Research found that only a small percentage of youth had evidence of nutritional referral, counseling, or prescriptions for medications to treat obesity.
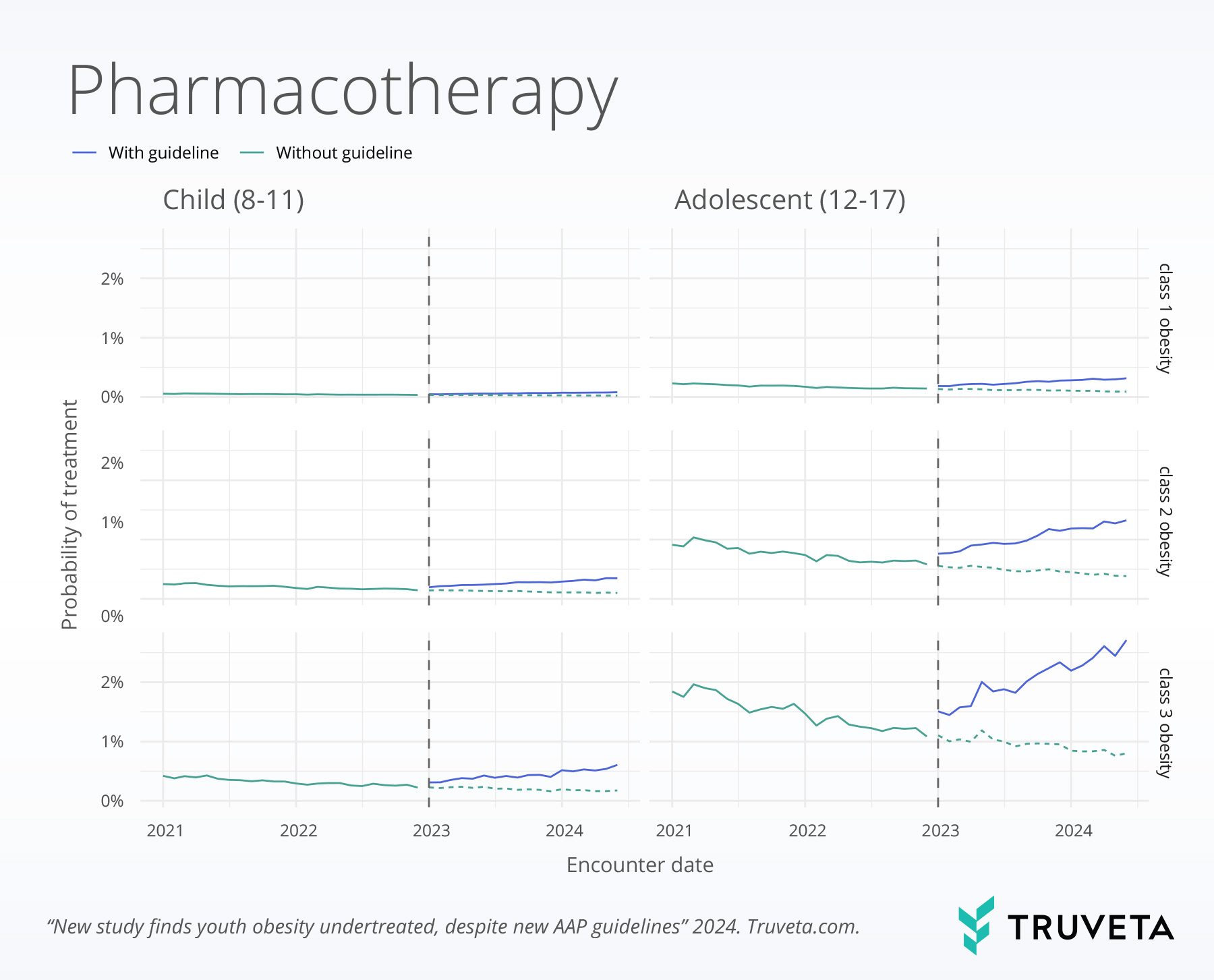
- While lifestyle interventions and prescriptions increased after the updated AAP guidelines, overall rates of obesity treatment remain low.
To explore the impact of these new guidelines, Truveta Research – in collaboration with Davene R. Wright, PhD, Harvard Medical School and Harvard Pilgrim Health Care Institute – has conducted a retrospective study to assess changes in obesity treatment practices for youth, examining trends in both lifestyle interventions and medication use since the AAP recommendations were introduced.
The full study is available on MedRxiv.
Key findings
Patient cohort
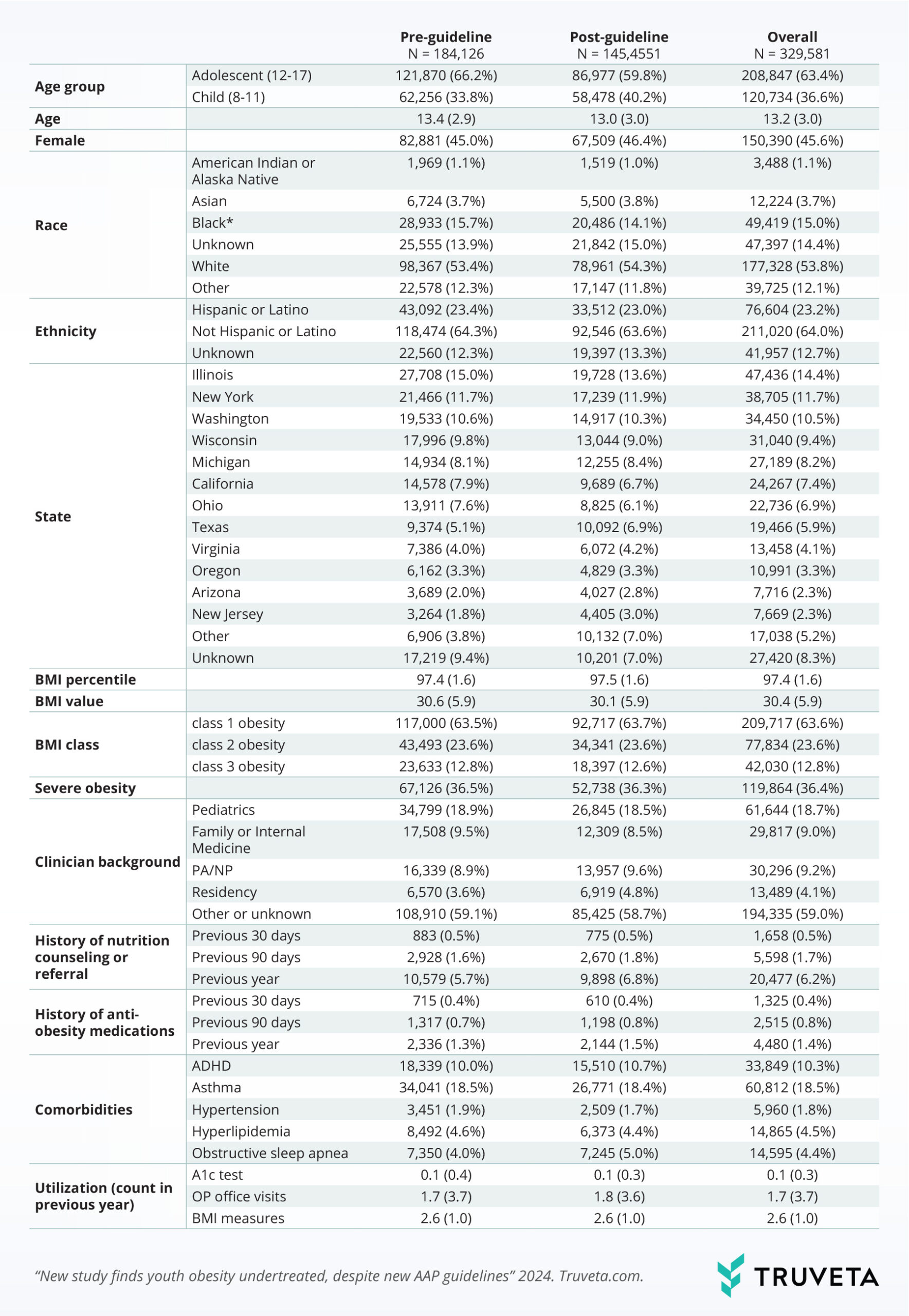
Adolescents aged 12-17 made up more than half of the study population (63%). The average age of the study population was 13 years, with nearly half (46%) of the patients being female and white (53.8%). The mean BMI percentile was 97.4, with 36% having severe obesity (class 2 or class 3).
For nearly half of the visits (47%), researchers had background information on the clinicians who saw the patients. Those visits were mostly with primary care professionals (87%).
The study evaluated treatment during two time periods: one before and one after the new guideline was introduced. Overall, patient demographics and health characteristics were similar across the two timeframes, though patients in the post-guideline period were slightly younger on average.
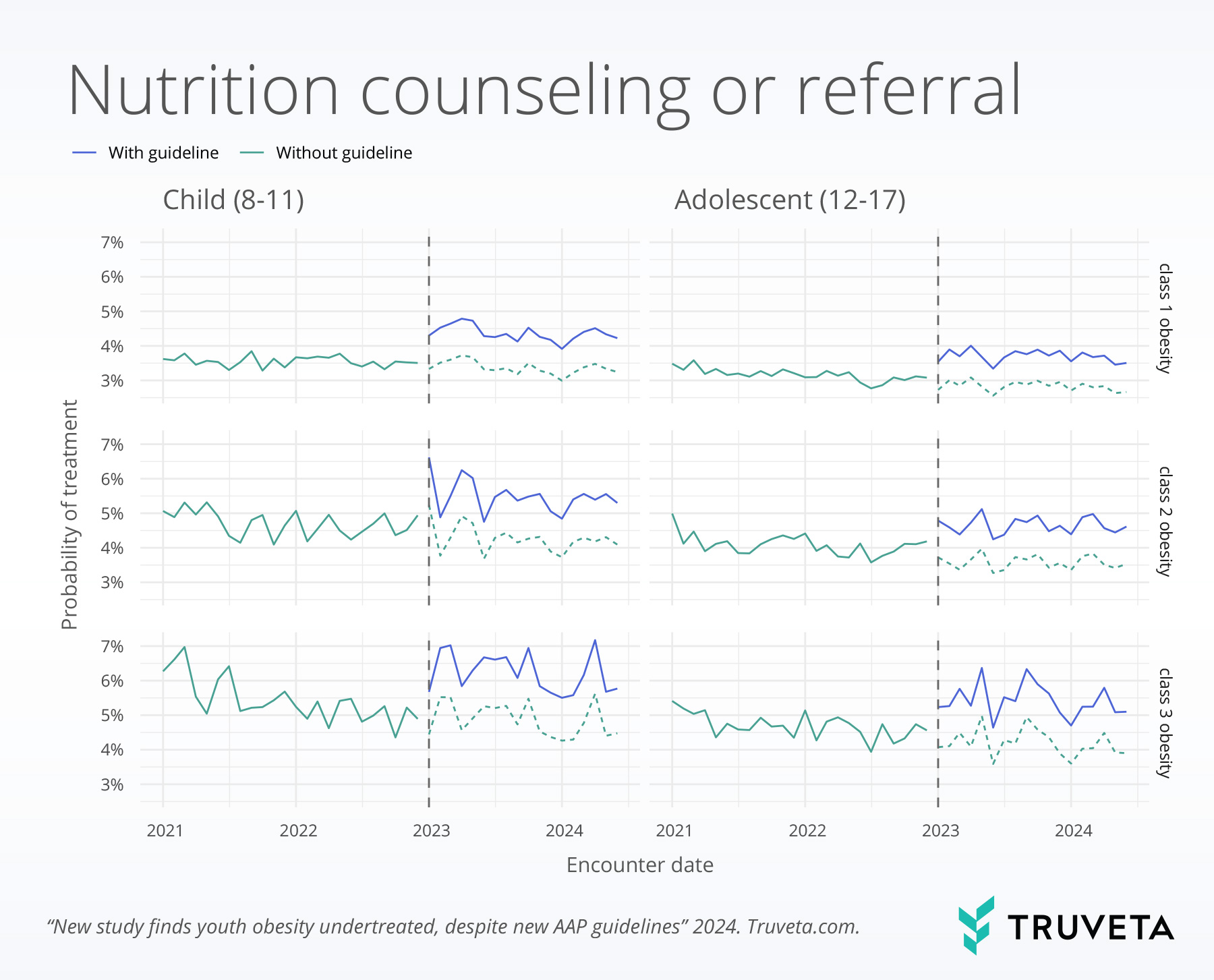
Nutrition referral or counseling
However, following new guidelines there was an immediate increase in treatment with nutrition referral or counseling (1.34% times higher), but no additional change in use over time since the guideline release.
Medications
After the new AAP guidelines, there was evidence of an immediate increase in the use of prescriptions (1.38 times) . Further, there was additional evidence of an increase in the monthly rate of medication prescriptions over time. Metformin was the most prescribed medication before the guidelines, accounting for nearly 82% of new prescriptions, while less than 2% of patients received semaglutide. Post-guideline, metformin prescriptions dropped to 68.5%, while semaglutide prescriptions rose to 20% for patients receiving a prescription.
Discussion
While the recommendation of anti-obesity medication for adolescents drew criticism about potential inappropriate overuse in youth, medication rates observed in this study stayed low. This aligns with other studies, which also show that medication use and obesity-related screenings are infrequent among youth. The higher prevalence of nutrition counseling may stem from concerns about medication safety, caregiver hesitancy, and limited insurance coverage for medications.
Barriers to youth obesity treatment include limited insurance, lack of time and social support, and stigma, as well as limited availability of effective lifestyle treatments. While research suggests strategies to reduce obesity, more focus is needed on supporting doctor-caregiver conversations about treatment, especially given social media and direct ads promoting anti-obesity drugs.
More research is needed on the safety of newer medications for adolescents. Continued monitoring of obesity treatment in children and adolescents is warranted given rapid changes in evidence, approvals, and access to evidence-based obesity treatments.
This study is also available in full on MedRxiv.