Case study
Reprieve and Truveta
De-risking clinical development and driving therapeutic innovation for heart failure
Heart failure (HF) impacts nearly 6.5 million Americans over the age of 20 in the US, with approximately 960,000 new cases each year. And HF readmission rates have worsened over the past decade. Optimizing acute inpatient decongestion is critical in mitigating HF morbidity and mortality, but few new treatment strategies have emerged in recent years.
With the most accurate source of RWD for HF being the nearly 20 year old ADHERE registry, Reprieve Cardiovascular needed immediate access to a contemporary, nationally representative real-world dataset with complete, patient-level data and rich clinical detail and came to Truveta.
Download this case study to see how they:

Identified a patient population 3x the size of the ADHERE registry.


Abstract
Contemporary Decongestion Strategies in Patients Hospitalized for Heart Failure A National Community-Based Cohort Study
Authors: Jimmy Zheng, MD, MS, Andrew P. Ambrosy, MD, Ankeet S. Bhatt, MD, MBA, SCM, Sean P. Collins, MD, MSC, Kelsey M. Flint, MD, MSCS, Gregg C. Fonarow, MD, Marat Fudim, MD, MHS, Stephen J. Greene, MD, Anuradha Lala, MD, Jeffrey M. Testani, MD, MTR, Anubodh S. Varshney, MD, Ryan S.K. W, BS, Alexander T. Sandhu, MD, MS
Background
Heart failure (HF) is a leading cause of hospitalization in the United States. Decongestion remains a central goal of inpatient management, but contemporary decongestion practices and associated weight loss have not been well characterized nationally.
Objectives
This study aimed to describe contemporary inpatient diuretic practices and clinical predictors of weight loss in patients hospitalized for HF.
Methods
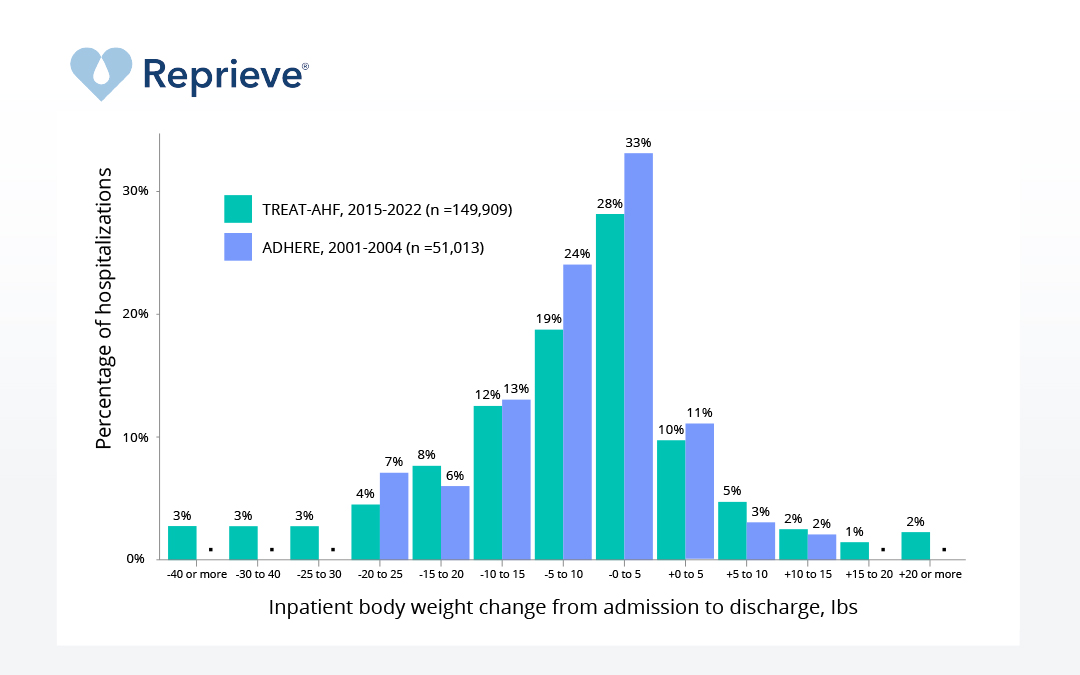
The authors identified HF hospitalizations from 2015 to 2022 in a U.S. national database aggregating deidentified patient-level electronic health record data across 31 geographically diverse community-based health systems. The authors report patient characteristics and inpatient weight change as a primary indicator of decongestion. Predictors of weight loss were evaluated using multivariable models. Temporal trends in inpatient diuretic practices, including augmented diuresis strategies such as adjunctive thiazides and continuous diuretic infusions, were assessed.
Results
The study cohort included 262,673 HF admissions across 165,482 unique patients. The median inpatient weight loss was 5.3 pounds (Q1-Q3: 0.0-12.8 pounds) or 2.4 kg (Q1-Q3: 0.0-5.8 kg). Discharge weight was higher than admission weight in 20% of encounters. An increase of $0.3 mg/dL in serum creatinine from admission to inpatient peak occurred in >30% of hospitalizations and was associated with less weight loss. Adjunctive diuretic agents were utilized in <20% of encounters but were associated with greater weight loss.
Conclusions
In a large-scale U.S. community-based cohort study of HF hospitalizations, estimated weight loss from inpatient decongestion remains highly variable, with weight gain observed across many admissions. Augmented diuresis strategies were infrequently used. Comparative effectiveness trials are needed to establish optimal strategies for inpatient decongestion for acute HF. (J Am Coll Cardiol HF 2024;-:-–-) Published by Elsevier on behalf of the American College of Cardiology Foundation